Using EyeGuide to monitor workplace fatigue in surgeon’s on 12hr and 24hr shift rosters
Article Type: SUS Society Paper
Section/Category: Clinical Research
Corresponding Author: Miss Beatrice Caballero, MS
Corresponding Author’s Institution: Texas Tech University Health Sciences Center
First Author: Yana Puckett, MD, MBA, MPH, MSc
Order of Authors: Yana Puckett, MD, MBA, MPH, MSc; Beatrice Caballero, MS; Theophilus Pham, MBA; Karen Castaneda, BS; Sharmila Dissanaike, MD; Robyn E Richmond, MD; Catherine A Ronaghan, MD Manuscript Region of Origin: USA
Abstract: Background: Visual tracking is the dynamic measurement of an individual’s visual attention and focus. In this quality improvement project, we analyzed surgeon focus and attention utilizing a visual tracking device. Our objective was to optimize surgeon scheduling to reduce surgeon fatigue thereby preventing surgeon burnout and reducing medical errors. We compared differences in focus after surgeons had completed a 12-hour in-house shift versus a 24-hour in-house call. We also compared focus scores between shifts among male and female surgeons and differences in focus between day and night shifts.
Materials and Methods: A prospective quality improvement project was performed on surgical residents and attending physicians (APs) working at a busy tertiary referral safety-net hospital with Level 1 trauma and burn centers. A visual tracking system was used to measure visual attention before and after a 12-hour in-house shift and a 24-hour surgical in-house call. A pupil tracker was utilized to measure attention impairment. Individual performance was rated on a scale of 0-6: Severely Impaired 0; Impaired 1; Low Average 2; Average 3; Above Average 4; High Average 5; Superior 6. Data was analyzed for homogeneity and Wilcoxon Ranked Sum was used to assess for statistically significant difference between focus scores in the same group of individuals before and after shifts/calls. Mann-Whitney U test was used to compare differences in focus between 12 and 24 hour in-house shifts/calls. Statistical Package for the Social Sciences (SPSS) Version 21 (SPSS, Chicago, IL) was used for statistical analysis.
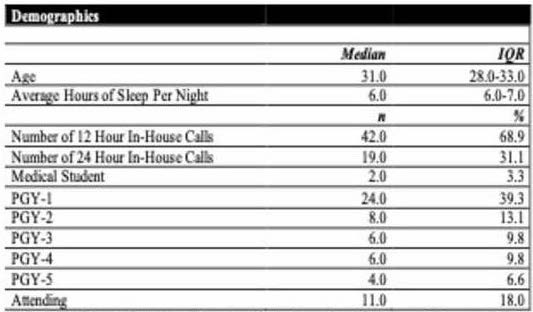
Results: A total of 21 surgeons provided a total of 61 visual tracking tests for analysis. Results were found to be nonhomogeneous. The project population was 46% men with a median age of 31 years IQR (28-33).
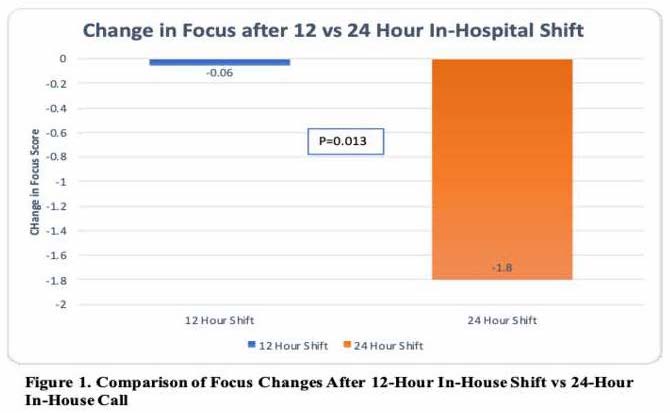
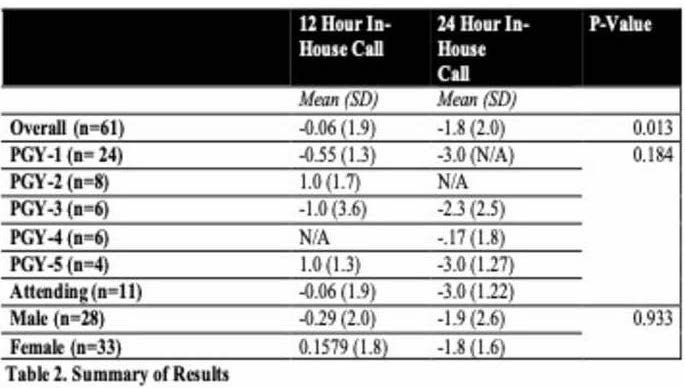
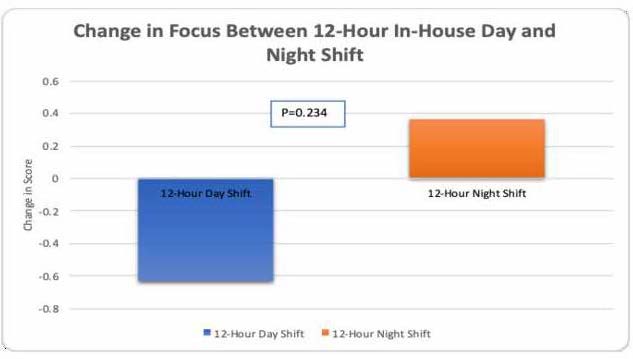
Residents accounted for 48 tests, medical students for 2 tests, and attending surgeons for 11. Average hours of self-reported sleep before the shift/call was 6 IQR (6-7). There was almost no overall change in focus in individuals before and after a 12-hour in-house shift -0.06 (SD 1.9) while focus dropped by almost two full grades -1.8 (SD 1.6) after 24- hour in-house call (p=0.013). Additionally, no significant difference was found in focus and attention scores between 12-hour day shift and 12-hour night shift. There was no significant difference in focus between male and female surgeons.
Conclusions: 12- hour in-house shifts appear to preserve focus in surgeons compared with 24- hour in-house calls. Changing call schedules to 12- hour in-house shifts may preserve visual attention skills and reduce surgeon fatigue.
Category of Manuscript is Surgical Outcome Research
This material has not been previously published or submitted elsewhere for publication and will not be sent to another journal until decision is made concerning publication by SURGERY.
No conflicts of interest, financial or personal relationships to disclose.
EyeGuide Focus device was provided to TTUHSC free of charge, with no arrangement to share data.
Authors
Yana Puckett, MD
Beatrice Caballero, MS
Theophilus Pham, MBA
Karen Castaneda, BS
Sharmila Dissanaike, MD
Robyn Richmond, MD
Catherine Ronaghan, MD
Department of Surgery, Texas Tech University Health Sciences Center, Lubbock, Texas
No sources of financial support
Corresponding author:
Beatrice Caballero
3016 26th Street, Lubbock, TX, 79410
Business Telephone number: (806) 743-2332
Home Telephone number: (520) 227-9016
Email: Beatrice.Caballero@ttuhsc.edu
Fax number: (806) 743-4031
Meeting: 14th Annual Academic Surgical Congress
Location: Houston, Texas
Dates: February 5-7, 2019
Surgeons Maintained Focus Working 12-Hour In-House Shifts While Experienced Severe Decline in Focus Working 24-Hour In-House Calls
Yana Puckett, MD; Beatrice Caballero, MS; Theophilus Pham, MBA; Karen Castaneda, BS; Sharmila Dissanaike, MD; Robyn E. Richmond, MD; Catherine A. Ronaghan, MD
Abstract
Background: Visual tracking is the dynamic measurement of an individual’s visual attention and focus. In this quality improvement project, we analyzed surgeon focus and attention utilizing a visual tracking device. Our objective was to optimize surgeon scheduling to reduce surgeon fatigue thereby preventing surgeon burnout and reducing medical errors. We compared differences in focus after surgeons had completed a 12-hour in-house shift versus a 24-hour in-house call. We also compared focus scores between shifts among male and female surgeons and differences in focus between day and night shifts.
Materials and Methods: A prospective quality improvement project was performed on surgical residents and attending physicians (APs) working at a busy tertiary referral safety-net hospital with Level 1 trauma and burn centers. A visual tracking system was used to measure visual attention before and after a 12-hour in-house shift and a 24-hour surgical in-house call. A pupil tracker was utilized to measure attention impairment. Individual performance was rated on a scale of 0-6: Severely Impaired 0; Impaired 1; Low Average 2; Average 3; Above Average 4; High Average 5; Superior 6. Data was analyzed for homogeneity and Wilcoxon Ranked Sum was used to assess for statistically significant difference between focus scores in the same group of individuals before and after shifts/calls. Mann-Whitney U test was used to compare differences in focus between 12 and 24 hour in-house shifts/calls. Statistical Package for the Social Sciences (SPSS) Version 21 (SPSS, Chicago, IL) was used for statistical analysis.
Results: A total of 21 surgeons provided a total of 61 visual tracking tests for analysis. Results were found to be nonhomogeneous. The project population was 46% men with a median age of 31 years IQR (28-33). Residents accounted for 48 tests, medical students for 2 tests, and attending surgeons for 11. Average hours of self-reported sleep before the shift/call was 6 IQR (6-7). There was almost no overall change in focus in individuals before and after a 12-hour in-house shift -0.06 (SD 1.9) while focus dropped by almost two full grades -1.8 (SD 1.6) after 24- hour in-house call (p=0.013). Additionally, no significant difference was found in focus and attention scores between 12-hour day shift and 12-hour night shift. There was no significant difference in focus between male and female surgeons.
Conclusions: 12- hour in-house shifts appear to preserve focus in surgeons compared with 24- hour in-house calls. Changing call schedules to 12- hour in-house shifts may preserve visual attention skills and reduce surgeon fatigue.
Keywords: physician fatigue; burnout; visual tracking; shift work; eyeguide focus
Introduction
Visual attention and focus is a significant component of patient assessment and treatment and is thus crucial in providing quality physician care,1,2 It is especially important in surgeons, who must utilize the oculomotor system to perform the task at hand. A decrease in attention and focus significantly affects workplace performance and learning, especially when tasks are dependent upon high levels of vigilance or newly learned procedural skills.
There are a number of expectations among surgical residents, including coming in early for a shift and staying late, working 24-hour in-house calls, performing a high volume of procedures and meeting multiple simultaneous deadlines. This is all anticipated to be performed at the highest level, while implementing sound, practical judgment, high-quality patient care, all in combination with specialized medical knowledge and training.3,4 Surgeons are subject to extensive work hours and sleep deprivation, both of which have an impact on focus and vigilant attention5. Undoubtedly, these are all qualities and hallmarks of a good surgeon and dedicated healthcare professional4. However, overwork can lead to counterproductive, unhealthy, or even self-destructive behaviors that may have negative repercussions for physicians themselves, their colleagues, their family, and their patients6-8.
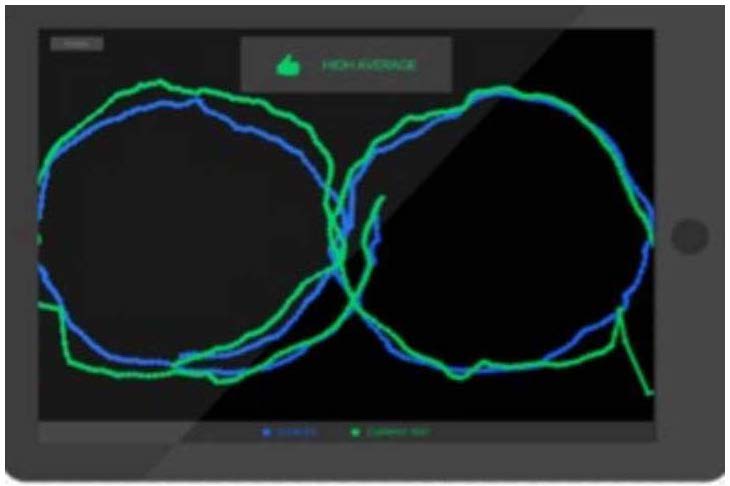
In this project, a visual tracking system is utilized to assess and compare attention and focus among surgical residents and attending physicians before and after both a 12-hour in-house shift and a 24-hour in-house call. The visual tracking system is a brain activity monitoring platform which provides fast, reliable measurements in 10 seconds. This eye tracking hardware was initially created to detect brain injury in young athletes, correlating traumatic brain injury with impaired performance on a smooth pursuit eye test, and is now implemented at multiple locations across the United States9,10. Scientific peer-reviewed literature features extensive studies which report on establishing the utilization of eye tracking visual stimuli to assess subject attention and cognitive performance 11,12.
The objective of this project was to determine optimal work schedules for TTUHSC Department of Surgery by quantifying differences in focus after surgeons had completed a 12-hour in-house shift versus a 24-hour in-house call. Focus scores between shifts among male and female surgeons and differences in focus between day and night shifts were also compared in order to identify any trends that could be used for improving surgeon scheduling.
Materials and Methods
Study Design: A single institution, quality improvement project performed on medical students, surgical residents, and attending physicians (APs).
Sample Size and Sampling: A total of 21 subjects volunteered and were tested for focus utilizing the visual tracker before and after a 12-hour in-house shift and a 24-hour in-house call over a 4-month period. Inclusion criteria were all surgical residents and attending physicians at the Texas Tech University Health Sciences Center Lubbock, Texas campus who were either on full 12-hour in-house shift or 24-hour in-house call. Exclusion criteria were all surgical residents and attending physicians who did not complete the test after their shift.
During a trial period at our institution to the trauma and acute care surgery (trauma ACS) model of care, we studied the effect of in-house call and in-house shift on visual attention and focus among surgeons. The program was in the transition period between a traditional 24-hour in-house call schedule and a trauma ACS model of 12-hour in-house shifts. Over the first two months of the project the majority of attending physicians and residents were doing 24-hour in-house calls. Over the last two months of the study, the trauma ACS model was fully established. This provided a unique opportunity to look at different call periods with the idea of determining the best work schedules to optimize patient care and physician wellness.
Implemented in July 2010, the trauma ACS model was designed to combine trauma and emergency general surgery divisions into one 12-hour in-house call service13. This new model replaces a traditional (TRAD) model in which non-trauma patients requiring emergency surgical care had to wait for the general surgeon on call, oftentimes resulting in a delay in evaluation and treatment of critically ill patients14. The trauma ACS model reorganizes the use of general care surgeons and trauma surgeons into one team of surgeons who work 12-hour in-house shifts, eliminating 24-hour on call duties.
Data Collection: The visual tracking hardware (EyeGuide, Lubbock, Texas, United States) utilized in this study consists of a head-mounted eye tracking device and a standard 9.7-inch iPad. The iPad runs EyeGuide’s propriety Focus app, which provides roster management. The eye tracking software communicates with the software running on the iPad over a secure Wi-Fi connection. In the EyeGuide Focus test, the stimulus is a white filled circle against a black background that is located at the center of the screen and moves clockwise through one cycle of a “lazy 8” path (Figure 6). Users who can visually keep steady, accurate attention on a moving object in their environment, characterized as Dynamic Visio-Motor Synchronization (DVS) by Maruta et al., likely do not suffer from impairment. However, if users with acceptable visual acuity cannot keep attention on a moving object in an accurate way, then this may be indicative of potential neurological impairment10.
Quality Assurance: At the conclusion of the 10 second test, the test administrator receives confirmation of a successful or unsuccessful test. If the test is successful, the subject’s normative, individual baseline score is recorded. If the test is unsuccessful, due to poor headset fit, head movement during testing or other technical reasons, the subject is re-tested. Classification score of the tests ranged from 0-6 (Severely Impaired 0; Impaired 1; Low Average 2; Average 3; Above Average 4; High Average 5; Superior 6).
The EyeGuide Focus normative data has been collected to establish baseline thresholds for normative data and impairment measurement scoring. Data continues to be collected into a cloud database and each new baseline test refines the norm, thus improving the accuracy of the thresholds for measurement. Baseline data; N = 849, Mean = 29633.0509, 95% CI =
(29012.6583, 30253.4435), SD = 9209.8389.
Statistical Analysis: Wilcoxon Ranked Sum was used to assess for statistically significant difference between focus scores. Mann-Whitney U test was used to compare difference in focus between 12-hour in-house shift and 24-hour in-house calls. A p-value of 0.05 was considered to be statistically significant. Statistical Package for the Social Sciences (SPSS) Version 21 (SPSS, Chicago, IL) was used for statistical analysis.
Results
A total of 21 surgeons were tested before and after a 12-hour in-house shift or 24-hour in-house call for a total of 61 completed before and after tests. Data was analyzed for homogeneity and was found to be nonhomogeneous. Males comprised 45.9%. Median age was 31 years IQR (28-33). Average hours of self-reported sleep prior to the shift/call was 6 IQR (6-7) (Table 1). There was almost no overall change in focus during a 12-hour in-house shift -0.06 (SD 1.9). Focus dropped by almost two full grades -1.8 (SD 1.6) after 24-hour in-house call (p=0.013)
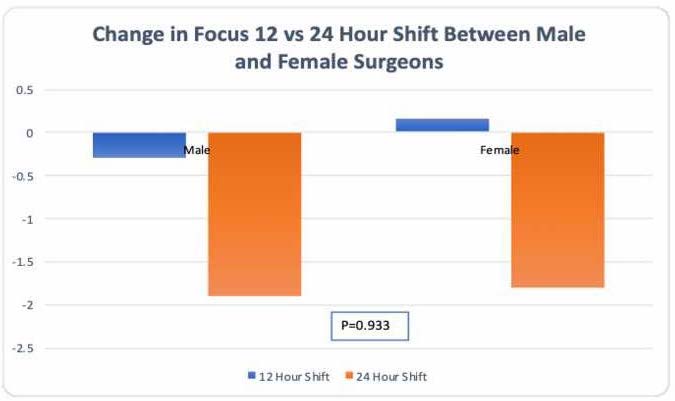
(Figure 1 and Figure 5), with the most impact seen among PGY5 residents and APs (Figure 2). There was no statistically significant difference in focus between a 12 hour and 24-hour in-house call between male and female surgeons (Figure 3). Additionally, no significant difference was found in focus and attention scores between 12-hour day shift and 12-hour night shift (Figure 4).
Discussion
To our knowledge, this is the first project to quantitatively demonstrate a significant decline in surgeon visual attention and focus after 24-hour in-house call. The findings have implications for both the surgeons’ well-being and performance.
We measured a baseline physiologic variable, removed from clinical context or opportunities to compensate for deficits. As such, the clinical relevance of these findings is debatable. However, it is quite likely to have an influence on tasks that require a high level of visual attention, such as performing an operation or rapidly interpreting a trauma CT scan. Visual attention has been used as a surrogate measure for cognitive function and levels of concentration15. Apart from the medical field, other fields such as aviation industry, require high levels of visual attention16.
One study revealed that visual fatigue is caused by overworking of the oculomotor system, which is responsible for an individual’s ability to focus and gaze whilst on duty15. Therefore, diminished alertness of the oculomotor system due to fatigue will cause an inability to focus and this in turn causes the surgeon to have reduced surgical performance, especially after working a 24-hour in-house call.
A different study reported that fatigue was linked to sleep deprivation and concluded that fatigue causes impaired learning, thought process and memory defaults17-19. Fatigue was a direct result of the surgeon working for 24 hours continuously, without taking a break. The study recommended that a mandatory 5-hour break should be undertaken in order to curb the extreme fatigue20.
Burnout is commonly experienced amongst medical practitioners due to unique stresses that come with the job. According to a study done on the prevalence, prevention and intervention of burnout amongst doctors, poor decisions are made when the level of burnout is very high. Furthermore, the study reported that doctors experiencing burnout were at higher risk of being hostile towards the patients and were also prone to making more medical errors due to poor judgement. The result of untreated burnout revealed depression and suicide amongst practitioners and concluded that prevention of burnout is more effective than treatment of burnout17. The current project focuses on a shift in the model from 24-hour in-house call to 12- hour in-house shifts. This change of working model is considered to be a preventive measure and could thus produce desirable results.
The lack of difference in our results based on the level of training of the surgeon was interesting; we had expected that more experienced surgeons would have evolved compensatory mechanisms after many years of taking 24-hour in-house call. As previously stated, we measured visual attention and focus stripped of clinical context. It is likely that surgeons do, in fact, learn to compensate for this post-call decline during their training to prevent adverse patient events, by taking longer to perform a procedure safely, for example. Previous studies in surgeons have shown a decline in cognitive performance, with relative preservation of technical ability, after 24-hour in-house call, which suggests there are mechanisms of compensation at play in these scenarios.
One study demonstrated that there was no effect on the cognitive performance after sleep deprivation, with no differences in relation to clear thinking, judgement, memory, and learning between different residents or the same resident but at different times. Thus, a conclusion was made that cognitive performance was only affected when surgeons were tired, however, this fatigue was not observed in all individuals21.
Another study concluded that resident fatigue is prevalent, pervasive and variable and found that 48% were fatigued and 27% were impaired during their time awake22. The study showed that the levels of fatigue varied, and thus visual disturbances could be assumed to be varied from the current study due to the variations in loss of concentration. A systematic review on surgeon burnout associated medical errors with burnout, suicide and depression23.
While surgeons may have evolved mechanisms to prevent this drop in visual attention from harming patients, there has been little research on the impact of 24-hour in-house call on the surgeons themselves. Several studies evaluated the effect of fatigue on focusing attention on a task at hand and processing incoming information. Subjects performed visual attention tasks continuously for extended periods of time without rest, which resulted in a decrement in their performance with increased simple reaction time and decreased visual tracking. These findings support that a decrease in visual attention can be closely associated with fatigue5,24,25.
Chronic fatigue is a risk factor for burnout, which is currently reaching epidemic proportions among physicians, including surgeons, in the United States. These findings suggest that 24-hour in-house call is a risk factor for fatigue, and frequent 24-hour in-house call likely has a significant impact on surgeon well-being. This is supported by a recent study by Jamie Coleman and colleagues in Denver, which revealed that the number of nights on call has been linked to physician burnout, which in turn is linked to depression and suicide. The replacement of individual daily in-house call pay with a team of surgeons hired to provide full time emergency general surgery coverage produced much better outcomes in terms of low burnout levels. This was achieved because the facility in question began employing the 12-hour in-house shifts for 14 days out of every 228 days, as well as 40 clinical workweeks blended between 12 hour in house calls and regular work days with shifts divided evenly among surgeons over a 1 year period. This model, therefore, allows surgeons to condense clinical work in 26 weeks while utilizing the rest of their time to conduct research and other non-surgical related jobs26.
One promising finding from this project is the preservation of visual attention and focus after 12-hour in-house shifts, even when the shift occurs overnight. This suggests a method to provide overnight coverage of high intensity services, such as trauma and acute care surgery that does not overly fatigue the surgeon. The trauma ACS model has been shown to benefit patient care and reduce healthcare costs by lowering length of stay and shortening time to surgery. A study by Kathleen B. To et al. reported that the ACS model was associated with a reduction of 31% in mortality in emergency general surgery27. The desired surgical outcomes of this model are in agreement with the reported benefits by the previous studies mentioned. This model also lends itself well to shiftwork, similar to that long adopted by emergency room physicians, who also work in a high intensity 24/7 environment.
This project was conducted during a time period where the authors’ practice group shifted to 12-hour in-house shifts and away from 24-hour in-house call for this very reason. After the transition, surgeons at our institution subjectively reported feeling less fatigued, more alert, and better rested. While anecdotal, these statements are congruent with the findings of this study, which measured one specific variable that is closely related to our ability to maintain focus and alertness.
Benefits of removing 24-hour in-house call include reassurance to the patient in emergency room that the surgeon is not fatigued while attending to them or an elective surgery patient is not inconvenienced by having the case rescheduled because the surgeon has to prioritize an emergency28,29.
Our project supports previous findings regarding lack of difference in visual attention and focus with age or gender. The national survey of burnout among US general surgery residents showed that women had higher burnout with high emotional exhaustion. Burnout reduced in those with structured programs26.
This quality improvement project was conducted at a busy Level 1 academic trauma and burn center with a large referral population for emergency general surgery; results may not be generalizable to other settings. This project includes variation in the surgeons who were assigned 12-hour in-house shifts versus 24-hour in-house call. Some residents and attendings participated in the project more often than others. There was no randomization to remove selection bias. Since this was based on the institutional call schedule and not random, it is possible that innate differences in visual attention between these individuals created bias in the results. To counteract this possibility, we are performing a follow-up study using within-person comparisons, so that each individual serves as their own control.
Conclusion
For too long, we have assumed that surgeons can compensate for the long hours of work. However, this project demonstrates objectively that such a compensation may be deleterious to quality of care provided to patients and well-being of surgeons. Thus, a movement towards 12-hour shift work versus 24-hour call may be warranted.
Acknowledgements
Authors’ contributions: Study design was done by Y.P., R.E.R., and C.A.R. Data collection was done by T.P., K.C., and B.C. Data analysis was performed by Y.P. Article drafting was done by Y.P., B.C., T.P., and K.C. Critical revision of article was done by Y.P., R.E.R., S.D, and C.A.R. No funding provided for this study.
References
- Arora S, Hull L, Sevdalis N, et al. Factors compromising safety in surgery: stressful events in the operating room. Am J Surg. 2010;199(1):60-65.
- O’Keeffe DA, Nugent E, Neylon K, Conroy RM, Neary P, Doherty EM. Use of a Novel Measure of Nontechnical Skills in Surgical Trainees: Is There an Association With Technical Skills Performance? J Surg Educ. 2018;00:1-7.
- Balch CM FJ, Shanafelt TD. . Stress and Burnout Among Surgeons. ARCH SURG. 2009;144:371-375.
- Akopov AL AD. Good surgeon: A search for meaning. Turk J Surg. 2017;33(2):49-50.
- Lim J, Dinges DF. Sleep deprivation and vigilant attention. Ann N Y Acad Sci.
2008;1129:305-322. - Campbell DA, Jr., Sonnad SS, Eckhauser FE, Campbell KK, Greenfield LJ. Burnout among American surgeons. Surgery. 2001;130(4):696-702.
- Bertges WY EA, Raoufi M, Aboulijoud MS. A National Study of Burnout Among American Transplant Surgeons. Transplantation Proceedings. 2005;37:1399-1401.
- Lebares CC, Guvva EV, Ascher NL, O’Sullivan PS, Harris HW, Epel ES. Burnout and Stress Among US Surgery Residents: Psychological Distress and Resilience. J Am Coll Surg. 2018;226(1):80-90.
- Kelly M. Technical Report of the Use of a Novel Eye Tracking System to Measure Impairment Associated with Mild Traumatic Brain Injury. Cureus. 2017;9(5):e1251.
- Maruta J, Tong J, Lee SW, Iqbal Z, Schonberger A, Ghajar J. EYE-TRAC: monitoring attention and utility for mTBI. Paper presented at: Sensing Technologies for Global Health, Military Medicine, Disaster Response, and Environmental Monitoring II; and Biometric Technology for Human Identification IX2012.
- Heitger MH, Jones RD, Macleod AD, Snell DL, Frampton CM, Anderson TJ. Impaired eye movements in post-concussion syndrome indicate suboptimal brain function beyond the influence of depression, malingering or intellectual ability. Brain. 2009;132(Pt
10):2850-2870. - Samadani U. A new tool for monitoring brain function: eye tracking goes beyond assessing attention to measuring central nervous system physiology. J Neural regeneration research. 2015;10(8):1231-1233.
- Hoyt DB, Kim HD, Barrios C. Acute care surgery: a new training and practice model in the United States. World J Surg. 2008;32(8):1630-1635.
- Britt RC, Weireter LJ, Britt LD. Initial implementation of an acute care surgery model: implications for timeliness of care. J Am Coll Surg. 2009;209(4):421-424.
- Reiner BI, Krupinski E. The insidious problem of fatigue in medical imaging practice. J Digit Imaging. 2012;25(1):3-6.
- Wu X, Wanyan X, Zhuang D. Pilot’s visual attention allocation modeling under fatigue. Technol Health Care. 2015;23 Suppl 2:S373-381.
- Kumar S. Burnout and Doctors: Prevalence, Prevention and Intervention. Healthcare
(Basel). 2016;4(3). - Landrigan. CP. Sliding Down the Bell Curve- Effects of 24-hour Work Shifts on Physicians’ Cognition and Performance. Sleep. 2005;28(11):1392-1402.
- Henrich N, Ayas NT, Stelfox HT, Peets AD. Cognitive and Other Strategies to Mitigate the Effects of Fatigue. Lessons from Staff Physicians Working in Intensive Care Units. Ann Am Thorac Soc. 2016;13(9):1600-1606.
- Ramsay MAE. Physician Fatigue. Proc (Baylor Univ Med Cent). 2000;13(2):148-150.
- Sturm L, Dawson D, Vaughan R, et al. Effects of fatigue on surgeon performance and surgical outcomes: a systematic review. ANZ J Surg. 2011;81(7-8):502-509.
- McCormick F. KJ, Landrigan CP, et al. . Surgeon Fatigue. A Prospective Analysis of the Incidence, Risk and Intervals of Predicted Fatigue-Related Impairment in Residents. ARCH SURG. 2012;147(5):430-435.
- Dimou FM, Eckelbarger D, Riall TS. Surgeon Burnout: A Systematic Review. J Am Coll Surg. 2016;222(6):1230-1239.
- Boksem MA, Meijman TF, Lorist MM. Effects of mental fatigue on attention: an ERP study. Brain Res Cogn Brain Res. 2005;25(1):107-116.
- Williamson AF, AM. Moderate sleep deprivation produces impairments in cognitive and motor performace equivalent to legally prescribed levels of alcohol intoxication. . Occup Environ Med 2000;57:649-655.
- Elmore LC, Jeffe DB, Jin L, Awad MM, Turnbull IR. National Survey of Burnout among US General Surgery Residents. J Am Coll Surg. 2016;223(3):440-451.
- To KB, Kamdar NS, Patil P, et al. Acute Care Surgery Model and Outcomes in Emergency General Surgery. J Am Coll Surg. 2018.
- Dissanaike S. Walking the Walk on Reducing Surgeon Burnout: How We Eliminated 24-Hour In-House Trauma Call. General Surgery News. 2018 45(12).
- Doyle C. Sleep Deprivation Common Among Acute Care Surgeons General Surgery News 2018 45(12).


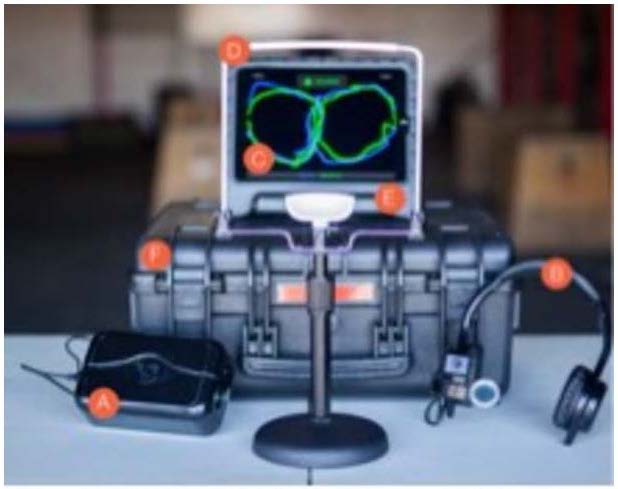
D. Headrest E. Tablet F. Storage box.
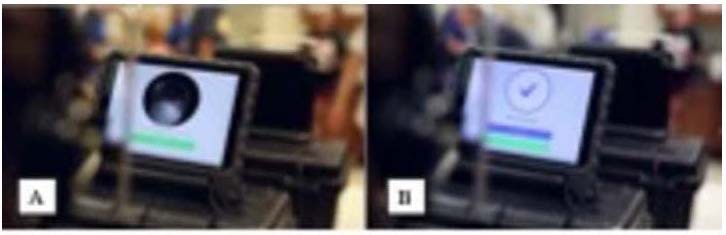
Figure 8B. Confirmation of successful test.